A processing report provides information on the status of the claim - whether it is to be paid in full, part paid, or rejected. For bulk bill claims, processing reports only exist when there is a problem with the claim or an adjustment needs to be made. For IMC claims, a processing report will always be generated whether or not any adjustments are made to the claim.
Processing reports are not retrieved from Medicare automatically. Rather you must request them. To do this a 'Status request' is first sent to see whether a report is available. If the Status request finds that a report is 'Ready' a separate request is sent to retrieve the report. These 2 processes can be done manually from any individual account, or they can be done in a batch process from the Eclipse Menu. Processing reports may be available as early as a few minutes after a claim is sent, or they may take some days.
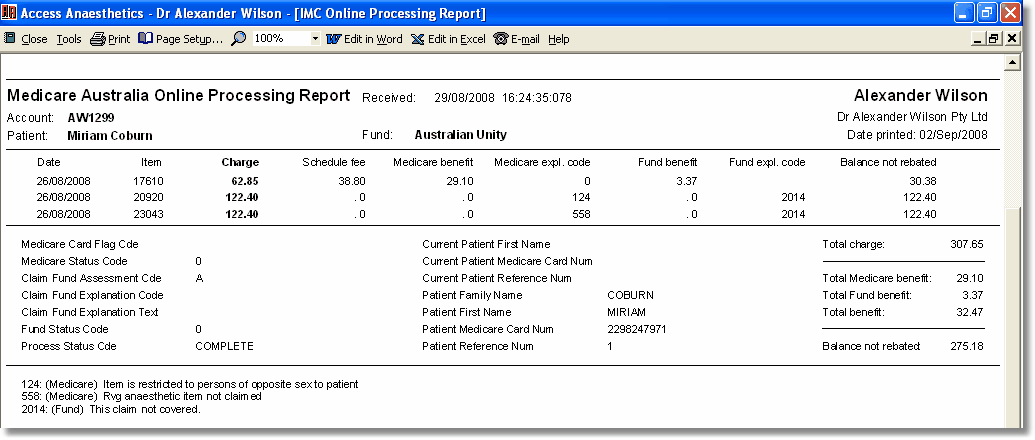
A processing report looks much like the Medicare benefit advice forms that you would be familiar with. There is a separate line showing details of each item claimed, the amount paid, and any explanation codes.
If a processing report indicates that the claim was rejected, or that no payment is due, the status of the claim will be set to Complete. Otherwise, retrieval of a processing report will change the claim status from 'Awaiting report' to 'Awaiting payment report'.
Retrieving a processing report also changes the account status. If the claim was rejected, the status is changed to Eclipse - rejected. If the claim was approved and the amount to be paid equals the fee charged, the status is changed to 'Payment approved-Eclipse'. All other processing reports will change the status to 'Review report - Eclipse'. These status changes enable the user to see at a glance what has happened to each of a group of accounts for which reports have just been received. On the Eclipse Menu, there are separate buttons to show accounts which are Approved, Rejected or Not fully approved.