An Inpatient Medical Claim (IMC) is a claim for treatment which is sent to Medicare and the Health Fund simultaneously. Medicare and the funds both evaluate the claim. Payment is made by the fund to the doctor and Medicare reimburses the fund for the Medicare rebate. This is the electronic equivalent to the no-gaps or known-gaps systems currently in place with health funds. You should set the fee for the account to the Health fund fee on the Fee page. If the fund accepts patient co-payments, you may also set a copayment fee which will be sent to the patient in the usual manner. The Medicare/Fund component can be claimed electronically.
IMC claims can also be made on behalf of the patient. This means that if the patient has paid the account in full, the practice can send an electronic claim for Medicare and fund rebates that will be mailed to the patient. This means the patient does not need to claim rebates independently. See Claim types for further details on IMC patient claims.
After entering the account details, click the Inpatient Medical Claim (IMC) button on the Eclipse tab to start the claim wizard.
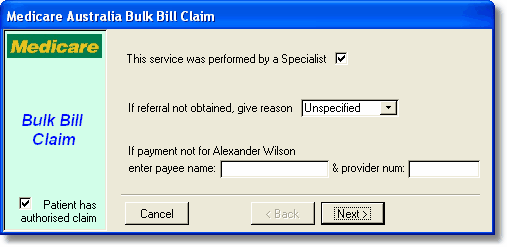
The referral and payee details on the first page follow the same rules as for bulk bill claims. |
|
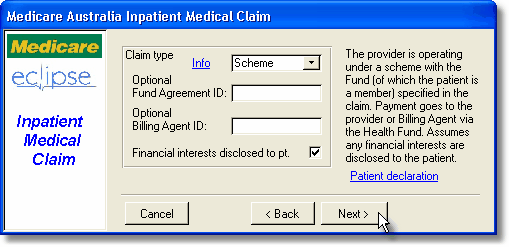
There are several types of IMC claim. The most common type is 'Scheme' and this will appear as the default.
A description of the claim type is shown on the right of the page, and you may click the <Info> button to display details about the other types of IMC claim.
For more details on the options on this page and the different claim types, click here. |
|
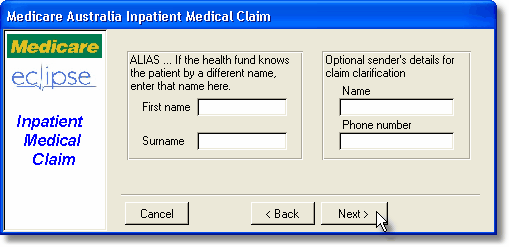
The final data entry screen for IMC claims allows entering an alias if the health fund knows the patient by a different name.
Also, the name and contact number of the person to call regarding enquiries about this claim can optionally be supplied. This would normally be the practice manager, billing secretary or individual provider. |
|
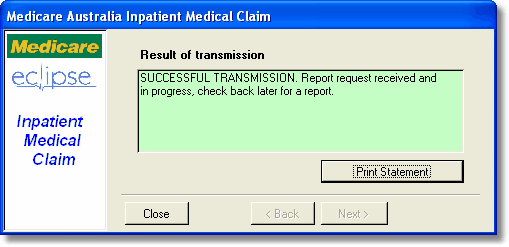
The claim details will be checked for errors. If any errors are found, you will be notified and should go back and correct them before creating the claim again.
Once there are no errors in creating the claim, click the <Transmit claim now!> button. If all goes well, after a few seconds you will receive confirmation that the claim has been transmitted successfully.
You may print a statement now if you like, although this is not required. |
|
After successful transmission of an IMC claim, the status of the claim will be set to 'Awaiting report', and the status of the account will be set to 'Awaiting payment - Eclipse'. Further management of the claim is done by retrieving reports.