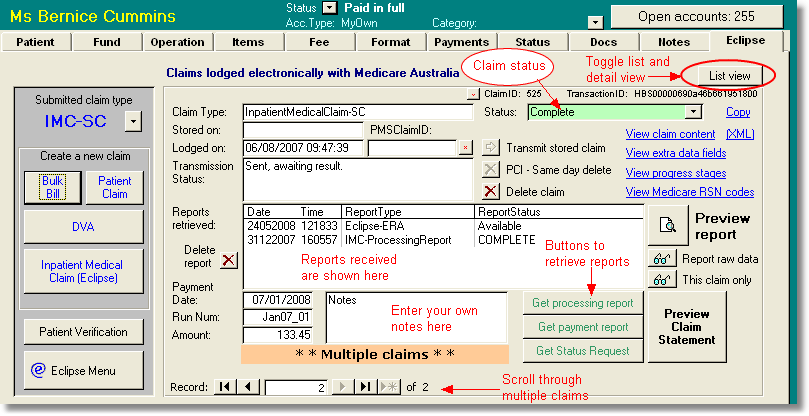
The Eclipse tab contains details on all the claims sent from to the current account. There may be multiple claims since even a patient verification process will create a claim record. Where there are multiple claims, you may scroll through them using the arrow buttons at the bottom left of the screen. Alternatively, you can view the claims in a list by clicking the <List view> button on the top right. Most data on this page cannot be edited directly.
ID Fields
The ClaimID is a field used by Access Anaesthetics to identify each claim. A button is provided to search by this ID field.
All claims have unique identifier (TransactionID) which is created by the Eclipse system and which is used to track the claim within the transmissions sent to and received from Medicare Australia.
The PMSClaimID is an additional unique identifier for bulk bill claims. A button next to the field allow searching for a specific PMSClaimID.
The <Copy> button on the top right will copy all relevant identification information to the clipboard so it can be pasted into an email or document for troubleshooting purposes.
Claim type
This is set by the system when a claim is created. Possible values are BulkBill (BB), DVAClaim (DVA), InteractivePatientClaim (PCI), SameDayDeleteRequest (SDD), PatientClaimStoreForward (PCS), InpatientMedicalClaim (IMC-AG/SC/MO/MB/PC), OnlinePatientVerification (OPV). It is assumed that only one claim type will be sent per account (excluding patient verifications). When a claim is created, the claim type will be displayed in the 'Submitted claim type' field on the top left. This field is shown in the List of Accounts in the 'Eclipse' column. More on claim types ...
Dates
If a claim is stored prior to transmission, a date will be shown in the 'Stored on' field. When the claim is sent electronically, its lodgement date and time will be recorded. The date and time that any report is received is recorded. This is used to identify the report.
Stored claims
Claims may be stored prior to transmission. Stored claims may be transmitted using the <Transmit stored claim> button near the middle of the screen. More commonly, stored claims will be sent in a batch from the Eclipse Menu. Claims that are transmitted without first being stored are automatically stored before transmission so that the details are retained if there are any transmission problems.
Retrieving Reports
Reports may be retrieved by clicking one of the 3 green report buttons. A processing report will provide details on whether the claim has been accepted for full payment, part payment or rejected. A payment report will show details of payments made. A status request will identify where the claim exists in the overall processing procedure. A list of the different stages is shown under the <View progress stages> button. Reports are available for retrieval for a period of 6 months after they were created. Rather than use these buttons, a more efficient report retrieval process is provided in the Eclipse Menu, where reports from multiple claims can be retrieved together.
Viewing Reports
When reports are received from Medicare Australia, they are displayed in the reports list. For most reports a formatted printout can be viewed using the <Preview report> button. The raw data for any report can also be viewed using the <Report raw data button>. Since some reports may contain data for multiple claims, an additional button allows viewing raw data which applies to the current claim only. The <Preview claim statement> button is intended mainly for bulk bill and patient claim claims. This will print a report formatted according to the specific requirements of Medicare. It is not likely to be used for standard IMC Medicare + Fund Eclipse claims.
Click here for full details on reports
Deleting claims and reports
Although claims may be deleted, we don't recommend this once a claim has been transmitted. Deleting the claim does not cancel it in the Online system, rather the claim is still recorded as active by Medicare and the health fund. Claims should only be deleted if they have been generated in error, and if the Medicare/fund processing has been completed (canceled/failed etc). A claim can only be deleted if there is not payment report. To delete such a claim, you must first delete the payment report independently. By contrast, deleting a claim will automatically delete any matching patient verification, status request or processing reports.
PCI claims. There is a special function for cancelling a transmitted PCI claim (Interactive Patient Claims). This is referred to as SDD or 'same day delete'. This function will send a transmission to Medicare to indicate that the transmitted claim should be canceled. These can only be deleted on the same day as they are transmitted. This cancels the transmitted claim, and inserts a record of the cancellation in the database.
Payment reports. Bulk Bill and ERA payment reports may be deleted, although we don't recommend this. Deleting the payment report will also delete the associated payments, including all components of batch payments (unless they are spread across multiple doctors). An additional prompt is provided before the payment is deleted, in case you need to retain the payment details after deleting the payment report. We anticipate this would only be necessary where a payment report had been duplicated. A claim cannot be deleted if a payment report exists; the payment report must be delete first.
Other reports. Patient verification claims (OPV) and reports may be deleted at any time since there is no real benefit to retaining this information. Status Request reports may similarly be deleted at any time, especially once a processing report has been received. Status Request reports may be deleted as a group by going to the Eclipse Menu > Setup > Maintenance.
Miscellaneous
<View claim content>. Allows viewing the content of the data that is being sent to Medicare for a particular claim. The data that is actually sent is encrypted and cannot be viewed in a readable format.
<(XML)>. Allows viewing the content of the data that is being sent to Medicare for a particular claim. The data is shown in XML format in a browser window. The data that is actually sent is encrypted and cannot be viewed in a readable format.
<View extra data fields>. Shows the data that is entered during the claim creation stage which is saved in a separate table and is only required for electronic claims. Some of this data may be edited, although this is not recommended.
<View progress stages>. Show the various stages that a claim will pass through from sending to completion.
<View Medicare reason codes>. Shows a list of Medicare reason codes and their meaning. These code will be returned with reports from Medicare when required. An additional set of return codes are used for Eclipse transactions. These can be viewed from the Eclipse Menu by clicking <View log>, then <Ret Codes>. These are for reference only - the explanation is always displayed alongside the code when printed on a report.